results found
IN THIS ARTICLE
You may have felt the echoes of weight stigma in some shape or form in your life. As a woman, preparing to enter into the reproductive phase of your life brings with it another layer of stigma.
Weight stigma describes the challenges that fat folx experience living in a world that has ingrained biases about weight and maintains barriers to everything from well-fitting clothing to adequate healthcare. This level of stigma shows up in full force in women’s reproductive health, with the effects manifesting well before a woman may choose to achieve pregnancy.
Weight stigma permeates the lived experiences of women, from those looking to support their fertility to postpartum and given the lack of research and evidenced based treatment for women’s healthcare overall, it’s important to know the facts for your own health in and out, babe!
Here’s some fact checking for you to take with you:
Fertility
- Women seeking or undergoing fertility treatments are often the target of weight stigma and shame as many clinicians will only provide treatments to those within a certain BMI range. But did you see our article of why BMI is actual bullshit? The reality is, these BMI ranges are arbitrary and non indicative of health status, what is true is that there are not large bodies of research done on fertility medications for those in larger bodies.
What you can do to fight it: Arm yourself with the research around weight and fertility and find a provider who will work with you to answer your questions, come up with creative solutions and advocate for the right treatment for your body that doesn’t just include “have more sex and lose weight” to get pregnant. Nicola Saloman has some wonderful resources on this topic as well.

Pregnancy & Birth
- During pregnancy, weight stigma is associated with increased rates of postpartum depression and greater weight retention at one year postpartum. Weight gain guidelines for pregnancy are based on pre pregnancy BMI (again, another false ruler) and women living in fat bodies are often assumed to have higher incidences of gestational diabetes, and even assumed to have more difficulty breastfeeding.
What you can do to fight it: Remember weight does not equate to health and that you can maintain a healthy pregnancy at any size. If you are looking for alternatives to monitoring weight through pregnancy, a health care provider can monitor what is known as your fundal height during pregnancy to monitor the baby’s growth. You can also elect to have your weight monitored “blind” which means that you can choose to step on the scale backwards and ask the number not to be shared with you.Maintaining health behaviors at any weight and actively protecting yourself against weight stigma and shame is the most proactive way to decrease the stress hormone (cortisol) and care for yourself and your baby during pregnancy. Plus Size Birth has a powerful collection of birth stories for women navigating birth choices living in a larger body.

Postpartum
- Postpartum messages surrounding “losing the baby weight” are palpable almost as soon as the baby is delivered, and echoes in the ears of women in fat bodies constantly after birth. In a culture fixated on bodies, the acceptability of weight gain during pregnancy compared to the immediate pressure to “return to normal” after birth is highlighted during this time. Larger breasts and bodies are falsely associated with lower milk supply and present more challenges during breastfeeding due to positioning.
What you can do to fight it: Your body was born to birth and breastfeed your baby – at any size. Breasts of any size can produce milk and adequately feed your baby. Although some creativity may need to be involved when positioning your baby at the breast, a skilled lactation consultant can help you achieve a comfortable position.
Protect your mental health through careful self-care and support, knowing that the pressure for weight loss can have worse impacts on your physical healing after birth, your milk supply & mental health overall. Connecting with a maternal mental health therapist and fat ally can be a wonderful outlet for support in processing your experience throughout.
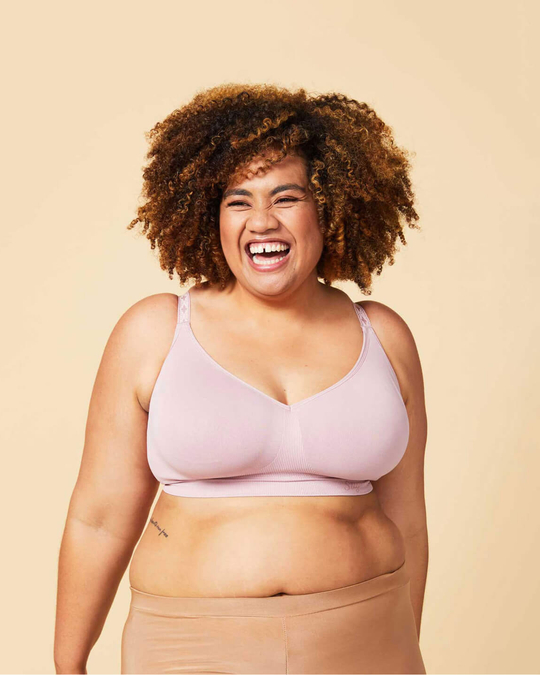
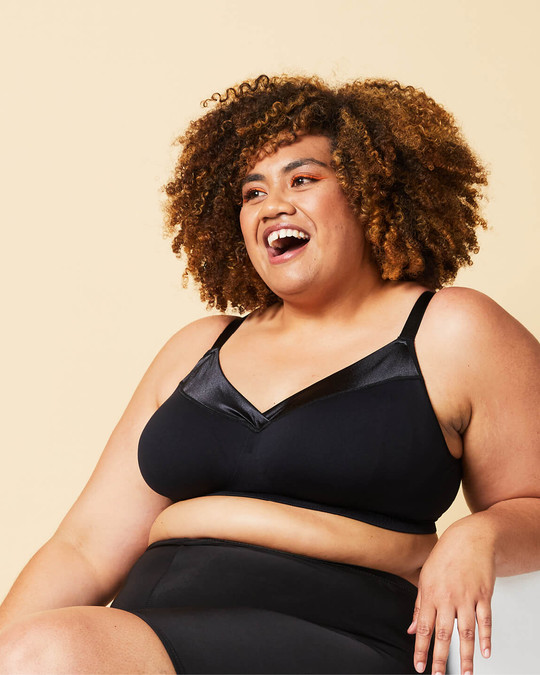
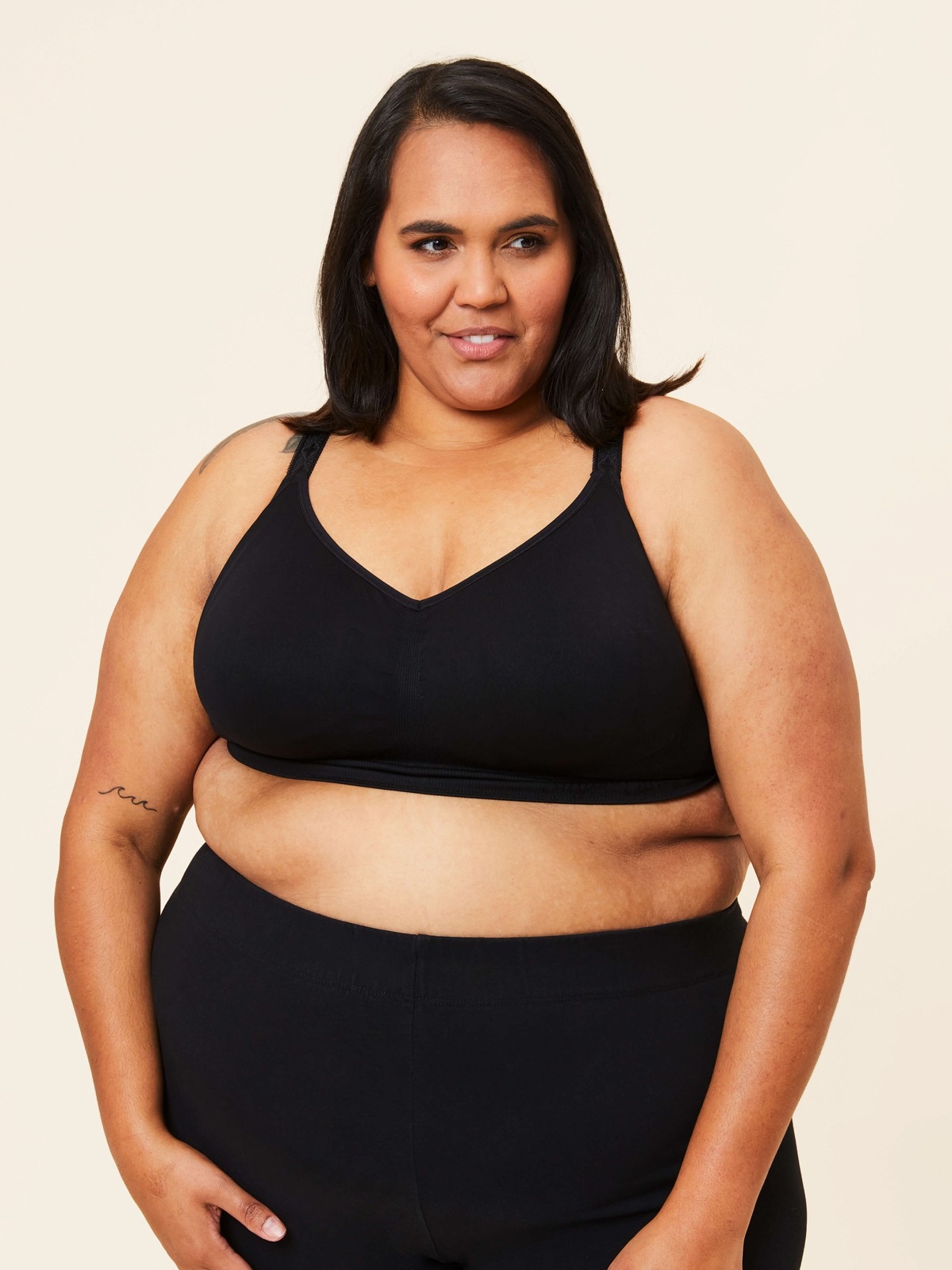
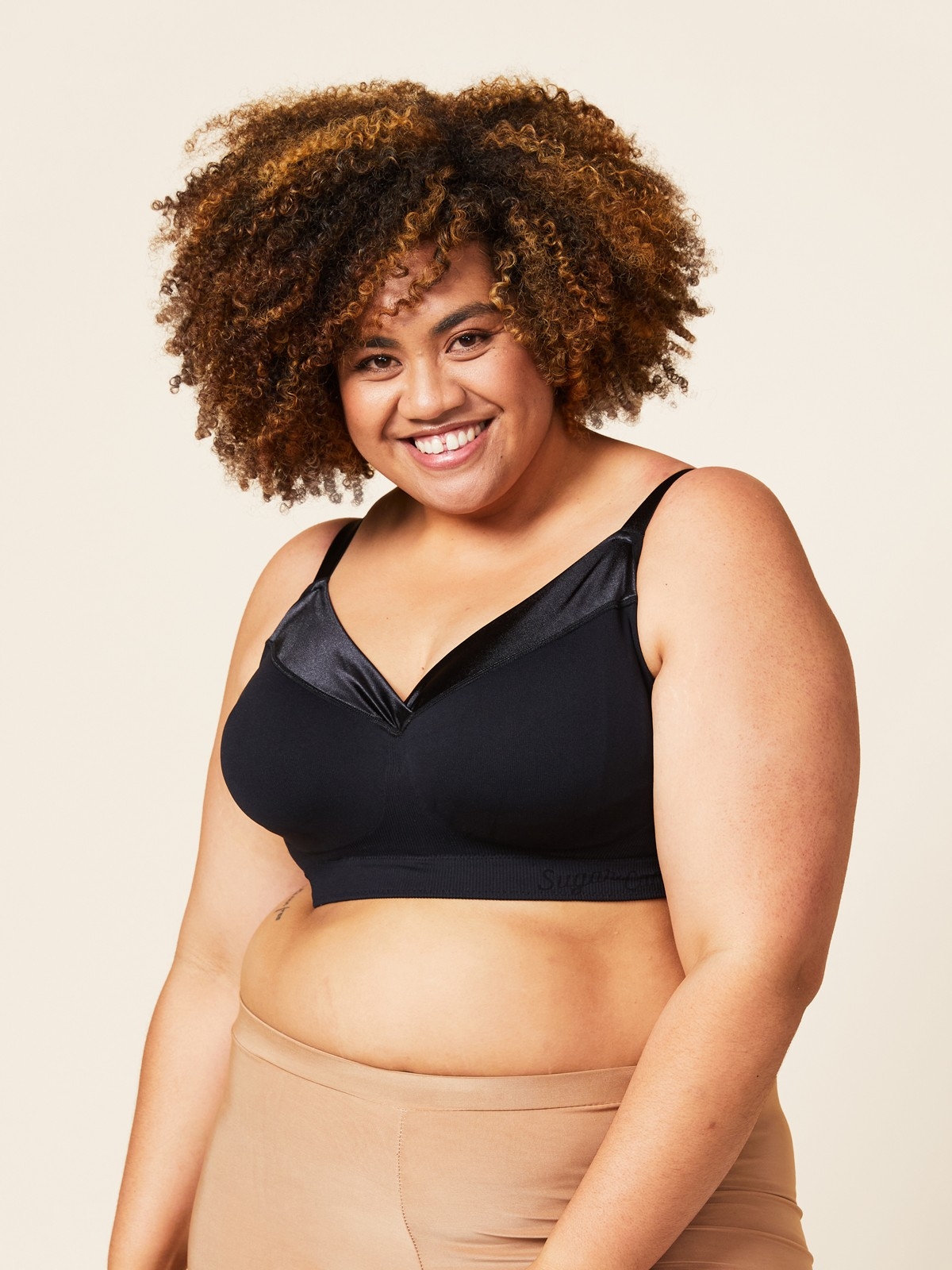
So here’s to more #boobpositivity and smashing the ideas that our bodies need to look or be a certain way in order to get pregnant, birth or feed a baby. We really CAN do it all. Armed with the right tools you can help create a new change to crush #weightstigma for each and every woman, by taking tremendously good care of yourself + advocating for change.

Jaren Soloff is a Registered Dietitian and International Board Certified Lactation Consultant (IBCLC) who serves as an expert in women’s health. While continuing to practice in the field of eating disorder treatment, Jaren gained additional experience as an IBCLC to fuse her love of nutrition and women’s health.
Now working solely in private practice, Jaren combines her expertise as a skilled nutrition therapist and lactation consultant to support individuals looking to heal their relationship with food and body. FULL CRCL provides evidenced based practices to support women at all stages of the reproductive cycle, from preconception to postpartum. Informed by her own journey and the hundreds of women she has counselled, Jaren’s experience comes full circle to support women in navigating pregnancy, birth and postpartum from a simple and intuitive framework.
WANT MORE SUGAR?
Sign up to our mailing list to get 10% OFF!
Plus you’ll be the first to hear about new releases, sales, promos and so much more when you join the club!
You might also like